Diabetic Ketoacidosis
Introduction
Diabetic Ketoacidosis (DKA) is a life-threatening diabetic emergency that consists of the biochemical triad of;
Hyperglycaemia (BM > 11)
Insulin deficiency leads to increased glucagon and glycogenolysis which causes hyperglycaemia
Ketonaemia (capillary blood ketones >/= 3)
Increased lipolysis leads to increase in fatty acids that are broken down to ketones
Acidaemia (pH < 7.3)
Accumulation of ketones cause metabolic acidosis
Hyperglycaemia, vomiting that is often associated with DKA and decreased PO intake can result in severe associated fluid and electrolyte derangement
DKA can occur in a known Type 1 Diabetic often secondary to an acute illness/infection or as in this case, it can be the first presentation of the disease.
Clinical Features
Symptoms
Nausea & Vomiting, Abdominal Cramps
Polyuria & Polydipsia
Lethargy, Fatigue
Symptoms of concurrent illness e.g. gastroenteritis, LRTI
Signs
Appearance
pale, lethargic, dry, ketotic smell on breath (pear drops)
Abnormal Vitals
Tachypnoea (Kussmaul’s Breathing)
Tachycardia, hypotension (if severe dehydration) altered conscious state, hypoxia = all indicate severe DKA
Oliguria/Anuria
Signs of concurrent illness e.g. chest sepsis etc
Complications
Cerebral oedema
esp in paediatrics due to overly quick correction of dehydration and electrolyte abnormalities
Severe Acidosis, severe hypokalaemia leading to arrhythmia and death
Acute MI or Stroke in older people
Differential Diagnosis
Other Causes of Metabolic Acidosis
Starvation or Alcohol Ketoacidosis
Lactic Acidosis
organ hypoperfusion or infarction, Liver injury
Toxins
e.g. methanol, ethylene glycol, iron, aspirin
Renal failure causing uraemia
Other Causes of Hyperglycaemia
Hyperosmolar Hyperglycaemic state
occurs in older pts. Normal pH & ketones
Endocrine
Steroids. Cushings disease. Glucagonoma,
Acute rise in BM due to other critical illness
Clinical Investigations
Bedside
Capillary BM + Ketones
helps make diagnosis and track response to treatment
VBG
low pH + bicarbonate. Confirms diagnosis. Low PCO2 due to respiratory compensation. High K. Low Na.
Patient will need hourly VBGs while being treated for DKA
Urine BHCG in all women of child bearing age
Urine dipstick
ketonuria. May be evidence of concurrent UTI
ECG
Changes due to High/Low Potassium. Evidence of Myocardial infarction
Laboratory
FBC – often a leucocytosis
U&E
AKI.
Potassium usually high initially due to acidosis and lack of insulin driving it into the cells. Drops quickly once treatment is started and patient will need K replacement
LFT, CRP & Blood cultures if ? sepsis as underlying source
MSU if ? urosepsis
Radiology
CXR if ? Chest sepsis
Other imaging as indicated by clinical condition
Management & Disposition
Initial Resuscitation
DKA patients should be managed in resus with close haemodynamic monitoring
Attention to ABC as clinically indicated
Specific Treatment
Following initial resuscitation the treatment priorities are;
Fluid Replacement
Insulin Therapy
Careful monitoring of potassium levels
Seek and treat any underlying illness
Every hospital has a DKA protocol. Follow it. Your aim is;
Fall in blood ketones of no more than 0.5 per hour
Maintain serum K within normal range
Avoid Hypoglycaemia
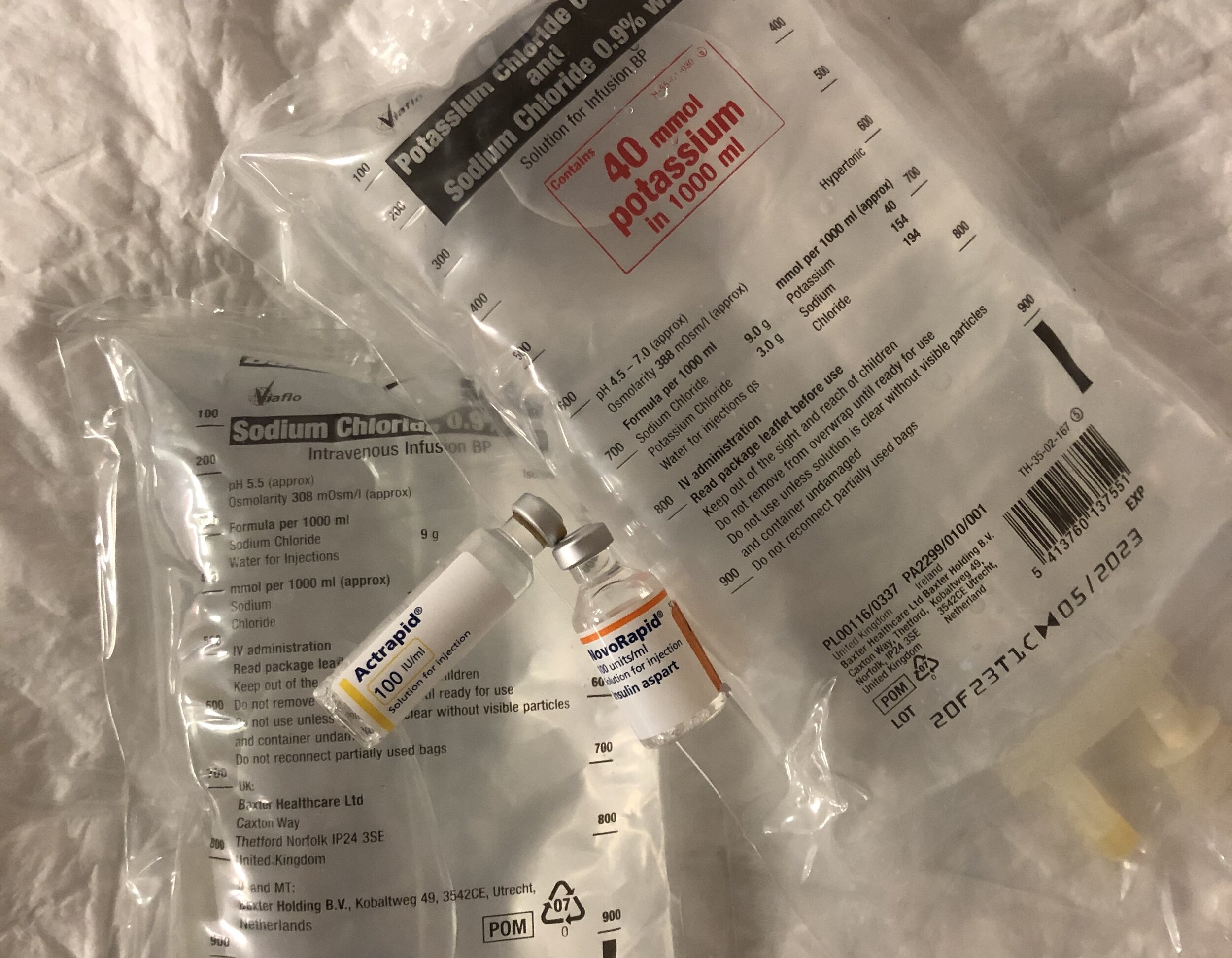
Fluid Replacement
1L 0.9% N Saline over 1 hour. Or faster if shocked
Will usually need at least another 3 L of N saline (+/- with K replacement) over next 8 hours
Insulin Therapy
IV infusion of short acting insulin (actrapid) titrated to blood sugar.
When BM is < 14 start concurrent IV Dextrose infusion as insulin infusion needs to continue until pH has normalised and ketones are cleared
Monitor Potassium Levels
Once Potassium is < 5mmol/L, 40mmol of KCL should be added to 0.9% N Saline infusion.
Max K infusion rate is 20mmol per hour.
Disposition
Endocrine Team should be involved early in all patients with DKA and these patients should ideally be admitted under their care
Severe DKA should be referred to critical care for admission to HDU until metabolic derangement resolves
References
Brown A, Cameron P. Chapter 11.2 Diabetic Ketoacidosis and Hyperosmoloar Hyperglycaemia State. Textbook of Adult Emergency Medicine. 4th Edition
SJH Prescriber Capsule. Endocrinology. Diabetic Ketoacidosis.
This blog was written by Dr Deirdre Glynn and was last updated in December 2020



