Haemoptysis
Introduction
Haemoptysis is the expectoration of blood, sometimes mixed with saliva or sputum, from the lungs or tracheobronchial tree.
There are many causes for haemoptysis (see below), however no cause is identifiable in around 30% of cases. A thorough history and exam should help to identify underlying causes.
Most patients present with small volume haemoptysis (< 20ml per 24 hours) and tend to be stable on presentation. A small percentage (~2%) present with massive haemoptysis which can quickly result in respiratory or cardiovascular compromise. Massive haemoptysis has a mortality rate of up to 80% and is defined as expectoration of a volume of blood that is significant enough to be life threatening by virtue of airway obstruction or blood loss. The most common causes of massive haemoptysis are lung malignancies and chronic inflammatory conditions such as TB, bronchiectasis and pulmonary abscesses.
Causes of Haemoptysis
It is important to differentiate haemoptysis from haematemesis, oral bleeding or nasopharyngeal bleeding i.e. that the blood was coughed up by the patient and is not from an other sources.
Pulmonary
Infection
Pneumonia
Tuberculosis
Lung Abscess
Bronchiectasis including cystic fibrosis
Neoplasm (primary or metastatic)
PE with pulmonary infarction
Trauma, foreign body
Connective Tissue Disease
Arteriovenous malformation
Extra Pulmonary
Oral e.g. dental, nasal or tongue bleeding
Pharyngeal e.g. Tonsillitis
GI Bleed
Cardiac
Acute pulmonary oedema/CCF
Mitral stenosis
Vascular e.g. aortic dissection
Bleeding disorders
Drugs e.g. Cocaine
Clinical Features
Symptoms
Infectious symptoms
cough, fever
Pain (often pleuritic)
Fatigue
Weight loss
Night sweats
Symptoms to suggest extrapulmonary causes e.g. recent vomiting, sore throat
Signs
May have nil of note to find on exam
Signs of airway obstruction
resp distress, stridor, gurgling respirations, hypoxia, cyanosis
Signs of shock
hypotension, tachycardia, altered conscious state, peripherally shut down
Respiratory signs
hypoxia, clubbing, tachypnoea, wheeze, crackles
Signs of systemic illness
pallor, cachexia
Signs of extra-pulmonary cause e.g. cardiac, abdominal, oropharyngeal signs.
Clinical Investigations
Bedside
Arterial Blood Gas (if Hypoxic)
?Respiratory Failure. Hb, Lactate, BM, Electrolytes
ECG
Cardiac cause for symptoms
Laboratory
FBC, CRP, blood culture if ?sepsis or infectious cause
Group and Hold/Crossmatch in severe cases
Coagulation screen
U&E,
Bone profile + LFTs
may show abnormalities in some malignancies
Sputum culture (If concerns regarding infection including TB) + Urinary antigens if ? pneumonia
not routinely done in ED but may be organised by admitting team.
Radiology
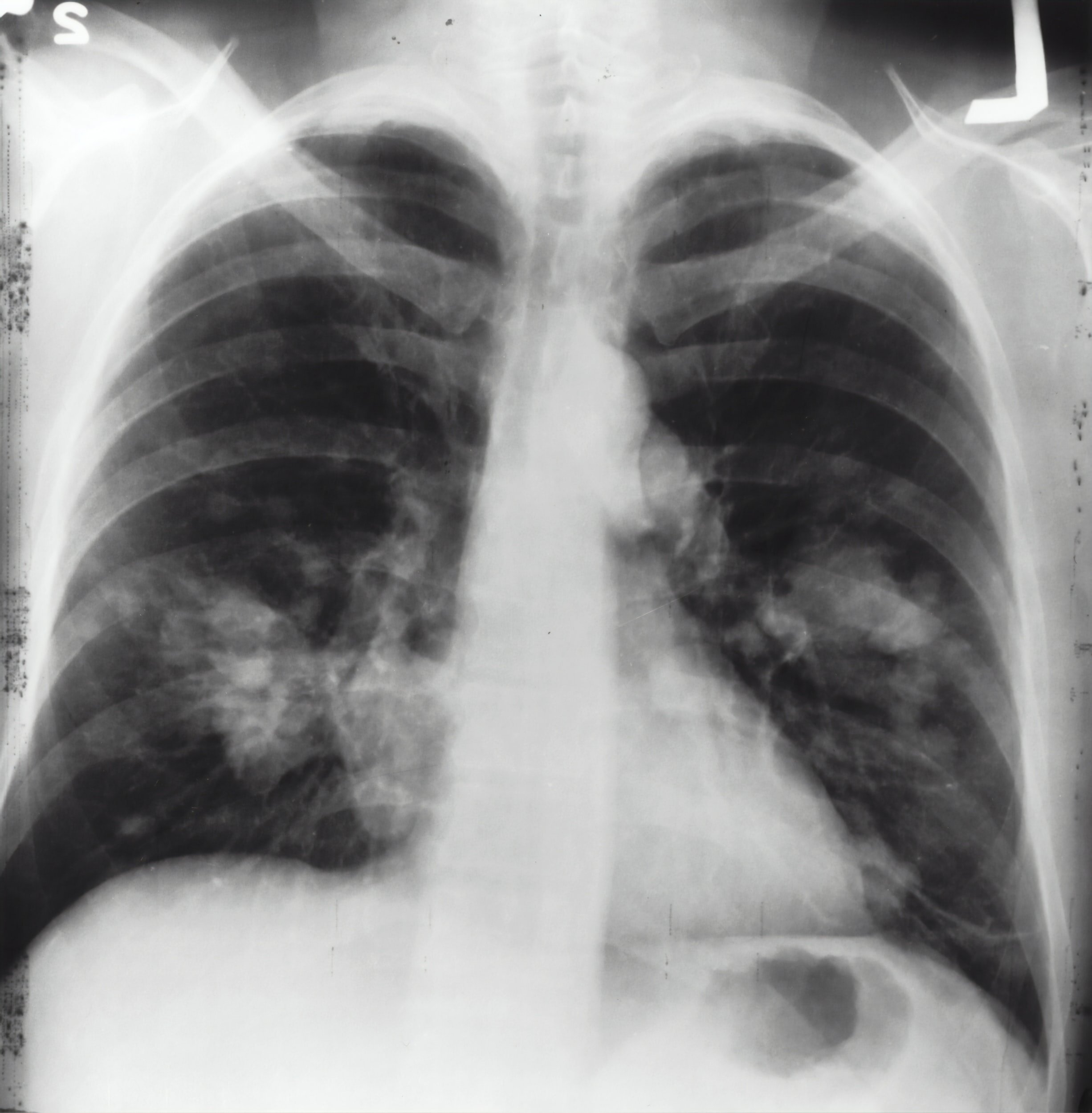
CXR
May identify an underlying cause. 20-30% will have normal CXR
CT
CT Thorax with contrast screening test of choice for ? malignancy, ? AVM, ? abscess. Further investigations may be needed to confirm diagnosis e.g. biopsy. IV contrast can demonstrate is there is active bleeding
CTPA if ? PE.
Bronchoscopy
Investigation of choice in cases where an abnormality of the bronchial tree is suspected
Direct visualisation and biopsy
In cases of massive haemoptysis therapeutic interventions can be done under direct vision via bronchoscopy as outline below.
Management & Disposition
Initial Resuscitation
Massive Haemoptysis
Resuscitation as required, following ABCs
nurse the patient lying on their side with the bleeding lung (if known) down, or in trendelenberg position
Airway compromise can occur quickly in massive haemoptysis
Suctioning & Oxygen as required for Sats >94%
Early intubation with large bore ETT if airway concerns.
consider double lumen tube if skilled operator and aware what side the lung pathology is
Declare CODE RED and commence warmed IV blood products if evidence of cardiovascular collapse
Specific Treatment
Massive Haemoptysis
Treatment depends on the patient and the source of bleeding
in those patients with advanced lung cancer invasive treatments may not be in their best interests.
Topical adrenaline or endobronchial balloon tamponade at bronchoscopy with respiratory physicians
Bronchial artery embolization with interventional radiology
Ongoing bleeding may warrant thoracotomy +/- partial or complete lobectomy with cardiothoracic surgeons.
Mild/Moderate Haemoptysis
Seek and treat underlying cause is generally only treatment required
e.g. antibiotics for infection, treat CCF etc
Disposition
Mild haemoptysis can usually be discharged from the ED with outpatient follow up
very important to have tight follow up. e.g. Rapid Access Lung Clinic if any possibility of underlying malignancy
Moderate haemoptysis should be admitted for inpatient work up and treatment of underlying pathology.
Massive haemoptysis patients if they survive initial insult will require ongoing airway and ventilatory management in ICU
References
Cham G ,Cameron P. et al. Chapter 6.8 Haemoptysis. Textbook of Adult Emergency Medicine. 4th Edition
Dixon J, Cline D. et al. Chapter 33 Haemoptysis. Tintinalli's Emergency Medicine Manual, 7th Edition
Case courtesy of Assoc Prof Frank Gaillard, Radiopaedia.org, rID: 8524
This blog was written by Dr Robert Evans and was last updated in February 2021




