Heart Blocks
Introduction
Heart blocks exist on a spectrum from the relatively benign 1st degree AV block to the serious 3rd degree or complete heart block as in this patients case. Heart blocks occur secondary to conduction abnormalities that can occur anywhere in the conduction system.
First degree heart block is defined as a PR Interval > 200ms (5 small squares). There is delay without complete interruption in conduction between the atria and ventricles. As an isolated clinical finding it is a benign entity and no specific treatment is necessary. It can occur as a normal variant in young athletes or those with high vagal tone. Though it may also be pathological.
Mobitz Type 1 second degree heart block (Wenchebeck) occurs when there is progressive lengthening of the PR interval until there is eventually a dropped ventricular beat due to failed conduction. The PR interval is longest immediately before the dropped beat and is shortest immediately after the dropped beat. It is usually a benign rhythm, causing minimal haemodynamic disturbance and with low risk of progression to third degree heart block
Mobitz Type 2 second degree heart block is a form of 2nd degree AV block in which there is intermittent non-conducted P waves without progressive prolongation of the PR interval. The PR interval in the conducted beats remains constant. The P-P interval is constant. The dropped beats may occur regularly as in 2:1 or 3:1 block or they may occur irregularly. Mobitz II is much more likely than Mobitz I to present with severe bradycardia, haemodynamic compromise and progression to complete heart block. It requires urgent cardiology opinion
Complete heart block (or 3rd degree heart block ) is a cardiac arrhythmia resulting from an abnormality in the cardiac conduction system in which there is no conduction through the atrioventricular node (AVN) leading to complete dissociation of the atria and ventricles. The atria and ventricles start beating independent of each other. Ventricular escape rhythm is visible which can arise from anywhere in the cardiac conduction system below the AV node.
Risk Factors for Heart Block
Cardiac
Cardiac Ischaemia
Idiopathic fibrosis of conduction system
Valvular heart disease
Inflammatory e.g. Myocarditis/Pericarditis, Rheumatic Fever, Lyme
Infiltrative Disease e.g. cardiac sarcoidosis, amyloidosis
Structural i.e. cardiomyopathy
Non- Cardiac
AV nodal blocking drugs e.g. CCB, Beta Blockers, Digoxin
Renal Failure
Electrolyte abns e.g. Hypokalaemia, hyperkalaemia, hypocalcaemia
Sepsis
Clinical Features
People with heart block may be entirely asymptomatic. Especially those with the relatively benign 1st degree and Mobitz Type 1 second degree.
Higher grade heart blocks i.e. Mobitz II second degree and complete heart block can present anywhere along a spectrum from entirely asymptomatic to critically unwell in cardiogenic shock.
Symptoms
Fatigue, lethargy
Light headedness
Pre-sycnope/Syncope
Chest pain
Diaphoresis
Generalised weakness
Signs
Signs of shock - hypotension, decr GCS, pallor, cool to touch, diaphoresis, confusion
Irregular slow pulse. Bradycardia
Low volume pulse
Clinical Investigations
Bedside
ECG
Assessing intervals, relationship between P wave and QRS complex, Number of P waves relative to QRS complexes
Signs of underlying causes e.g. ischaemia
VBG
acid base balance, K, Na, Ionized Ca.
POCUS
in shocked patient can be useful in narrowing down cause e.g. cardiomyopathy, regional wall motion abnormality, pericardial effusion
Laboratory
FBC & CRP
elevated acute phase reactants could indicate infection/inflammation
Urea & Electrolytes
Hyperkalemia, Hypokalaemia, Hypomagnesiemia, Hypocalcemia
Troponin
? Acute myocardial infarction
Radiology/Other
CXR
? signs of cardiac failure, ? infection
Echocardiography
pericardial effusion, Cardiomyopathy, RWMA, Valvular disease
CT Coronary Angiogram/Cardiac MRI
might be indicated depending on underlying cause and at the discretion of cardiology but are not indicated in the emergency department.
Management & Disposition
Just like any other arrhythmia, when you encounter a patient with complete hear block there are 2 questions you need to ask yourself.
Is the patients stable or unstable?
Is there a treatable underlying cause?
Initial Resuscitation
Unstable Patient
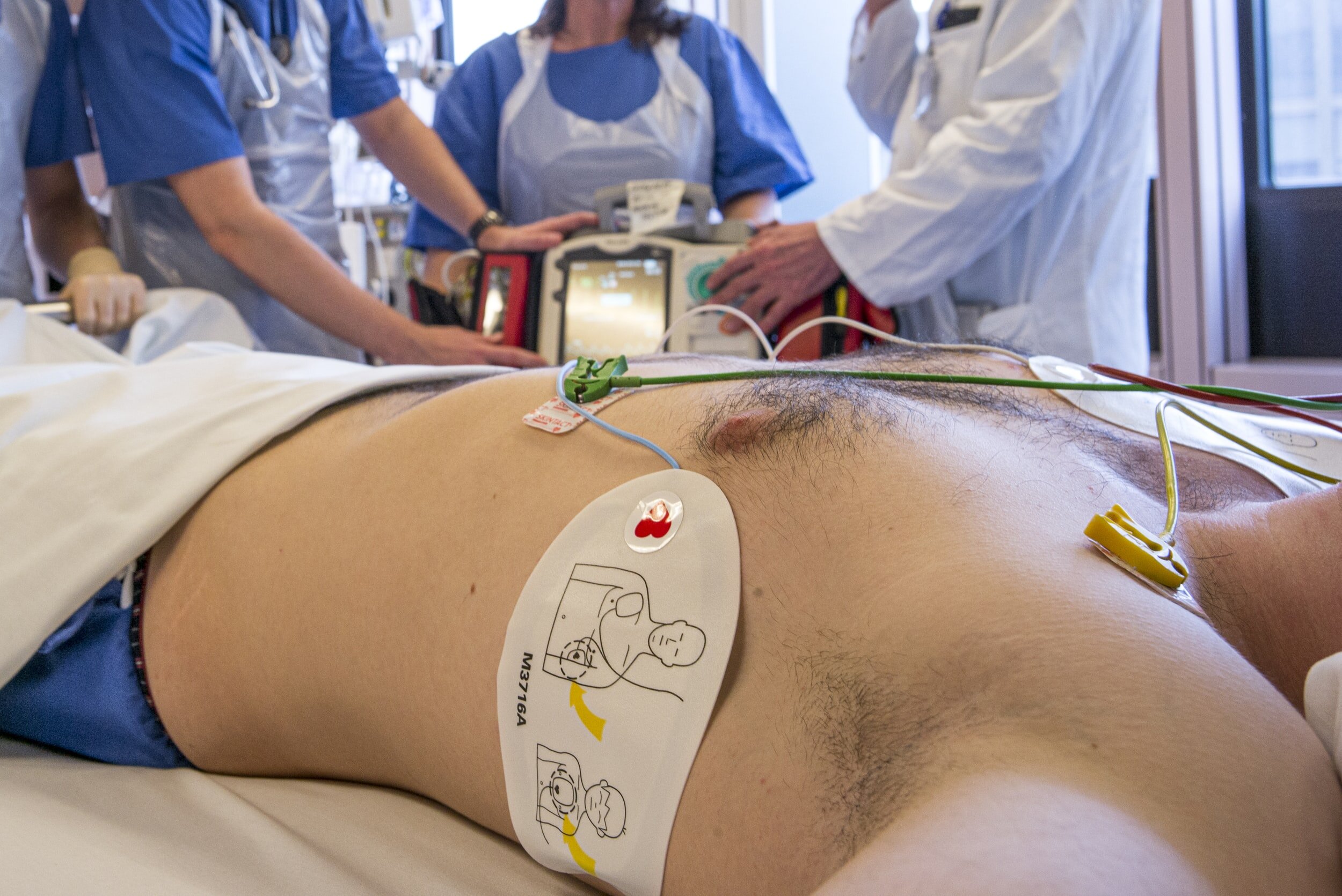
patient should be managed in resus with full non invasive cardiac monitoring
patient should be attached to the Defibrillator
3 lead ECG to sense the rhythm
Pads to transcutaneously pace if needed
Urgently seek and treat underlying causes e.g. correct electrolytes, activate cath lab if evidence of STEMI
Atropine 0.5mg
every 3-4 minutes to a maximum of 3mg in the unstable patient. Decreases vagal blockade at AV node. Rarely works
If patients clinical condition allows patient can be started on infusion of chronotropic drugs to increase heart rate e.g. dopamine, isoprenaline, adrenaline.
Transcutaneous pacing if pharmacological treatment fails or if patient is too unstable to wait for infusion preparations.
Specific Treatment
Seek and treat underlying cause
Transcutaneous pacing can only be continued for a short period of time due to patient discomfort and risk of burns.
should be converted by cardiology to transvenous pacing with a pacing wire as soon as possible
Those patients who present with Mobitz II 2nd degree and complete heart block who do not have a readily reversible cause will require urgent cardiology input and likely insertion of a permanent pacemaker
Disposition
Incidental finding of 1st degree AV block or Mobitz type I (Wenkebach) can generally be safely discharged to the care of their GP from ED if no other issue.
may require OPD cardiology follow up
Higher grade blocks will need to be admitted to a monitored area under the cardiology service +/- consideration for PPM
References
Kusumoto et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society.
This blog was written by Dr Mustafa Mehmood and last updated in February 2021







