Unstable Angina/NSTEMI
Introduction
Acute coronary syndrome (ACS) is a term used to describe a range of conditions resulting from sudden reduction in coronary blood flow. The presence or absence of ST-segment elevation on presenting ECG indicates ST-elevation MI, or non-ST – elevation acute coronary syndrome (NSTE-ACS).
NSTE-ACS is further sub-divided into NSTEMI (non ST-elevation myocardial infarction) or Unstable Angina, depending on elevation of troponin.
NSTEMI: ECG does not show persistent ST elevation, but may show ischaemic changes such as ST depression or T-wave inversion. The ECG may also be normal. Serum troponins are elevated.
Unstable angina (UA): Is present in patients with ischaemic symptoms suggestive of an ACS and a normal troponin, with or without ECG changes indicative of ischaemia (ST-segment depression or new T-wave inversion). It is largely a clinical diagnosis
Since an elevation in troponin may not be detectable for up to 4-8 hours after symptoms onset, UA and NSTEMI are frequently indistinguishable at initial evaluation. The importance of serial troponins cannot be over emphasised.
Risk Factors
Modifiable Risk Factors
Elevated cholesterol levels
Smoking
Hypertension
Diabetes mellitus
Obesity
Physical inactivity
Cocaine use
Non Modifiable Risk Factors
Atherosclerosis – History of angina, myocardial infarction, stroke, transient ischaemic attack, peripheral vascular disease.
Age > 65yrs
Male sex
Family history - MI in 1st- degree relative <55 years
Chronic kidney disease
Clinical Features
Symptoms
Pain
Chest pain that may radiated into the shoulder, arm, jaw, neck, or back.
Discomfort that feels like tightness, squeezing, crushing, burning, choking, or aching.
Pain that may have previously occurred only on exertion that now occurs at rest or minimal exertion and does not easily go away with nitrates = Unstable angina
Pain brought on by less activity, more severe, more prolonged or increased frequency than previously = Sometimes referred to as “crescendo” angina implying infarction is imminent.
Associations
Shortness of breath, sweating, nausea, pre-syncope, palpitations, belching, indigestion, fatigue
Signs
Most patients with non-ST elevation ACS will have a nil acute on physical exam
Assess for signs of modifiable risk factors. e.g. hypertension, hypercholesterolaemia
Signs of heart failure
Hypoxia, increased WOB, tachypnoea, 3rd or 4th heart sound, gallop rhythm, basal creps, elevated JVP
Differential Diagnosis
Cardiac
STEMI
Angina pectoris
Pericarditis
Myocarditis
Gastrointestinal
GORD
Gastritis
PUD
Oesophageal spasm
Cholecystitis/Biliary Colic
Vascular
Aortic dissection
Musculoskeletal
Costochondritis
Precordial catch syndrome
Trauma
Respiratory
Pneumothorax
Pulmonary embolism
Pneumonia
Neuropathic
Herpetic Neuralgia
Cervical Neuropathy
Clinical Investigations
Bedside
ECG
12 lead ECG and interpretation within 10 mins of arrival to ED to out rule STEMI which is a time critical, life threatening diagnosis.
dynamic ST-segment deviation (>0.5mm), or new T wave inversion (>2mm)
ECG may be normal or show minor changes in up to 50% cases.
VBG
acid-base status. ? high BM in poorly controlled DM
Laboratory
Serial Troponins
Used to distinguish NSTEMI (high troponin) from unstable angina (normal troponin).
Levels usually begin to rise around 2 -3 hours after onset of myocardial ischaemia.
Therefore serial troponins over at least 6 hours is necessary to out rule NSTEMI
Levels peak at approx 18 hours post pain and remain elevated for 14 days
FBC
Hb measurements may help to evaluate a secondary cause of NSTEMI (i.e., acute blood loss, anaemia)
? thrombocytopenia to estimate risk of bleeding.
U&E
? underlying CKD. Baseline renal function prior to commencing meds
K/Mg/Ca
Electrolyte derangements may predispose to cardiac arrhythmias.
Radiology
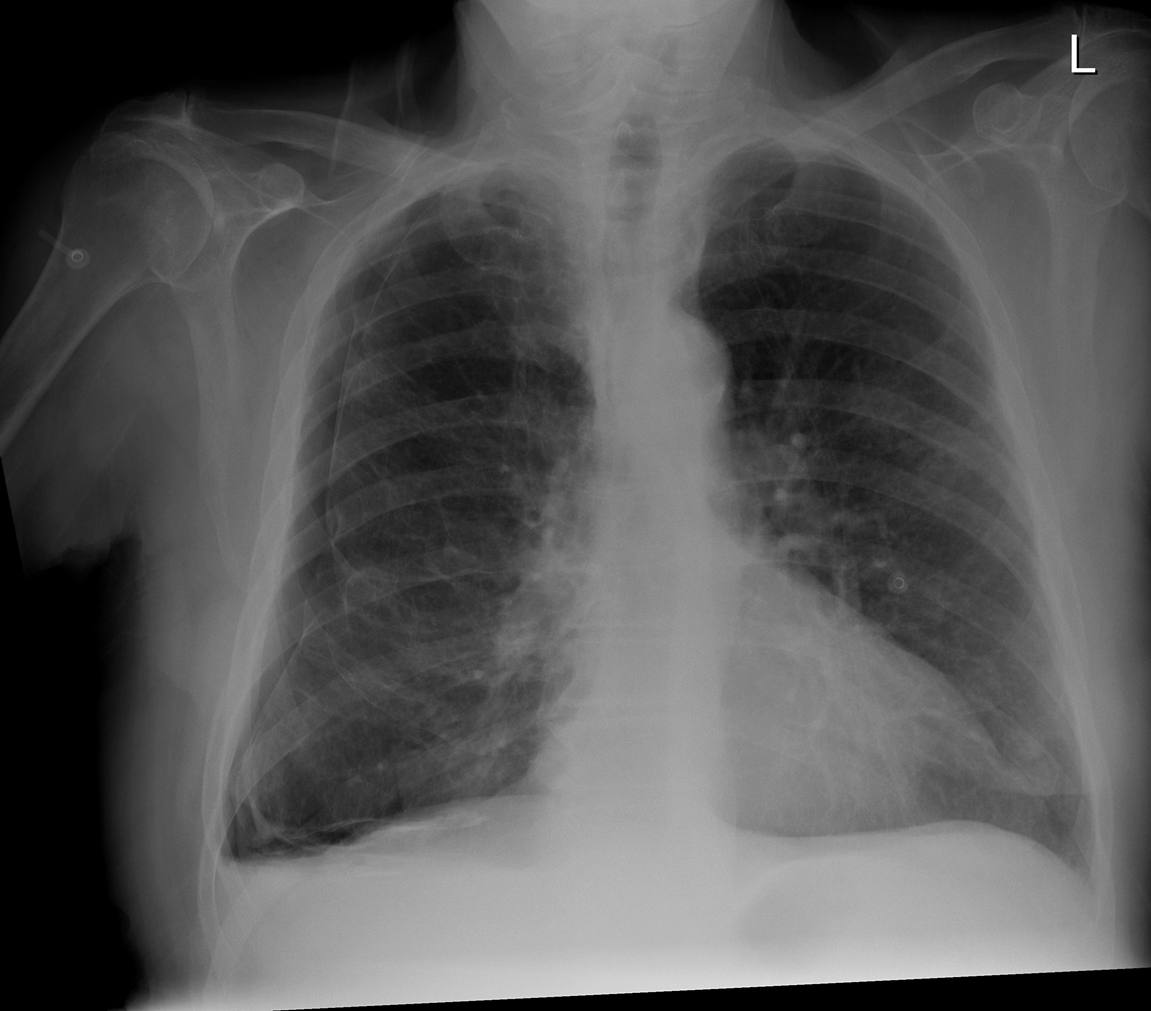
CXR
Assess for other diagnoses.
Assess for signs of heart failure
Echo
? regional wall motion abnormality
Evidence of underlying heart disease e.g. LVF, LVH
Management and Disposition
Initial Resuscitation
ABC as clinically indicated
O2 to keep sats > 92%
Specific Treatment
In ED give a loading dose of dual anti-platelet therapy (Aspirin plus P2Y12 Inhibitor)
Aspirin 300 mg PO
Ticagrelor 180 mg PO
Consider Beta Blocker if BP and heart rate allow to decrease myocardial work load
Symptomatic Treatment
Analgesia PRN in the form of IV Opioid +/- sublingual nitrate
Anti-emetic PRN
Disposition
NSTEMI and Unstable angina patients need to be reviewed by and admitted under the cardiology service for in patient angiography
CCU bed with continuous cardiac monitoring
References
1. B Wilkinson I, Raine T, Wiles K, Goodhart A, Hall C, O’Neill H. (2017) Oxford Handbook of Clinical Medicine. Oxford, UK: Oxford University Press.
2. Faselis C, Lieber J, Noto F. (2017) Step 2 CK Lecture Notes 2017: Internal Medicine. New York, US: Kaplan Medical.
3. https://bestpractice.bmj.com/topics/en-gb/151
This blog was written by Dr Maria Garcia and was last updated in Nov 2020