Spontaneous Pneumothorax
Introduction
Pneumothorax means air in the pleural cavity. Pneumothoraces are either spontaneous, traumatic or iatrogenic in origin. Traumatic & iatrogenic pneumothoraces will be dealt with elsewhere. From here on we will discuss only spontaneous pneumothoraces on this page.
Spontaneous pneumothoraces are generally split into two groups, primary spontaneous pneumothoraces which are pneumothoraces which occur in patients without underlying lung disease, and secondary spontaneous pneumothoraces which occur in patients with underlying lung diseases such as COPD or TB.
Risk Factors
Smoking is strongly associated with the development of pneumothoraces and pneumothoraces in non-smokers are exceedingly rare (1).
Risk factors for development of pneumothoraces include;
Smoking, both cannabis and tobacco
Genetic predisposition.
Secondary pneumothoraces are associated with a number or underlying lung diseases including (2);
COPD
Tuberculosis
Cystic fibrosis
Necrotising lung infections ie: PJP
Lung malignancies
Thoracic endometriosis
Clinical Features
Spontaneous pneumothoraces range in presentation from small apical pneumothoraces in patients with no underlying lung disease causing little or no symptoms, right up to tension pneumothorax which is a life-threatening emergency requiring immediate intervention.
Generally speaking patients with secondary spontaneous pneumothorax tend to be more symptomatic than those with primary pneumothoraces and patients with secondary pneumothoraces tend to be more compromised with relatively smaller pneumothoraces due to their reduced lung reserve.
Symptoms
Shortness of breath – the symptom which best correlates with the size of the underlying pneumothorax
Pleuritic chest pain
Dry cough
Signs
Respiratory compromise – the degree of compromise depends on the size on the pneumothorax and severity of underlying lung disease
Tachypnoea
Accessory muscle use
Low sats
Reduced air entry
Hyper-resonant to percussion
Tachycardia
Tension pneumothorax
Elevated HR, low BP
Distended neck veins
Tracheal deviation
Differential Diagnosis
Respiratory
Pulmonary embolism
Pneumonia
Exacerbation of COPD / asthma
Cardiovascular
Pericarditis
Myocardial infarction
Other
Musculoskeletal pain - this is a diagnosis of exclusion
Clinical Investigations
Bedside
12 lead ECG
May be normal or show sinus tachycardia in pneumothorax
Useful to rule out other differentials, ie pericarditis
Arterial blood gas if O2 sats are low, otherwise venous gas is adequate
Shows degree of hypoxia
May show hypercapnia & acidosis if significantly compromised
Point of care lung ultrasound – rule in investigation
Inter-operator variability reduces usefulness
Most commonly used in trauma patients who must remain supine and will show
Absent lung sliding
Absent B-lines
Barcode sign on M mode
Presence of transition point
Laboratory
Laboratory investigations are not that useful in the initial diagnosis and management of spontaneous pneumothorax however they are useful in ruling out other causes and in patients with concomitant problems such as infection.
FBC
May show elevated WCC – non-specific
CRP, U/E, LFT’s, Coag screen, troponin
Useful to rule out other differentials
Radiology
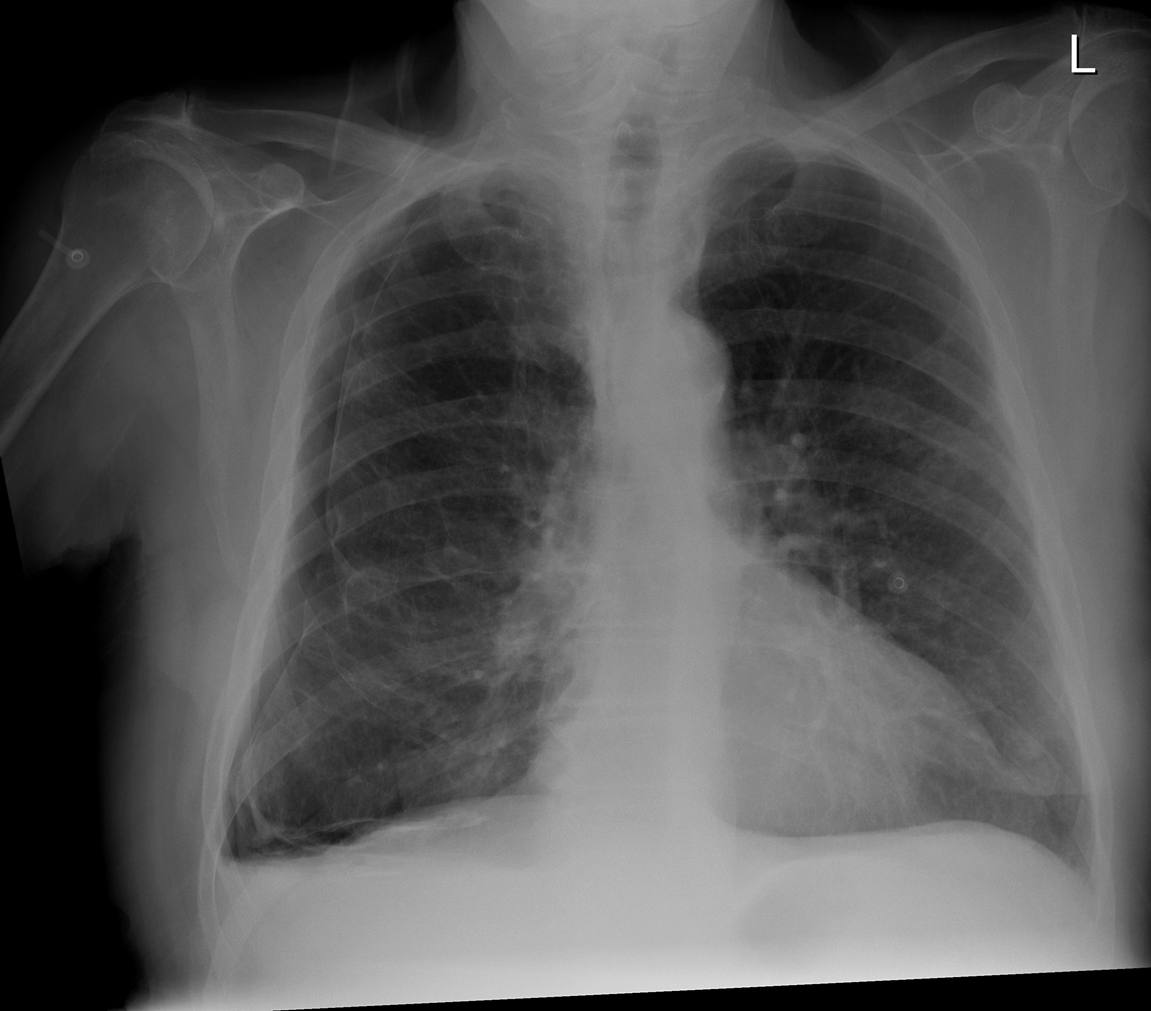
Chest x-ray
Initial investigation of choice due to ease of access
Difficult to accurately quantify the size of pneumothorax on chest x-ray
Large bullae may mimic pneumothoraces. If any doubt about the diagnosis CT thorax should be performed
Small apical pneumothoraces sometimes may be missed on traditional chest x-rays
CT Thorax
Considered gold standard for diagnosis and size estimation
Useful to rule in or out alternative diagnoses including bullae which can sometimes mimic pneumothorax
Management & Disposition
Haemodynamically unstable patients should be assessed and managed with a standard ABC approach. Patients who are haemodynamically unstable because of a tension pneumothorax should have immediate needle decompression followed by urgent chest drain insertion.
The traditional approach to needle decompression is insertion in;
Anterior chest wall
Mid-clavicular line
2nd intercostal space
Just above the inferior rib (avoids intercostal bundle)
Recently there is some debate of the best location for decompression however that is beyond the scope of this blog
Stable patients should be managed in accordance with the British Thoracic Societies guidelines on the management of spontaneous pneumothorax. The advice differs depending on whether the patient has a primary or secondary pneumothorax.
Any patients who are discharged from the ED either with no intervention or after aspiration of spontaneous pneumothorax should be given careful written and verbal discharge advice and should be booked into an clinic, ideally within 1 week for repeat x-ray and follow-up.
Discharge advice should include advice about
Planned follow-up
What to do if they become more unwell
Advice on what to avoid until planned follow-up;
Avoid Scuba diving (lifelong advice)
Avoid flying until pneumothorax has fully resolved
References
MacDuff A, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax. 2010; 65(18).
Light RW, Lee G. Pneumothorax in adults: Epidemiology and etiology. [Online].; 2020 [cited 2020 October 25. Available from: https://www.uptodate.com/contents/pneumothorax-in-adults-epidemiology-and-etiology?search=spontaneous%20pneumothorax&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1.
This blog was written by Dr. Emer Kidney and was last updated in November 2020





