Pyelonephritis
Introduction
Urinary tract infections are very common especially in women. It is more common in women who are older or who are sexually active. In males occurrence of UTI is very rare after infancy. As men get older and have increasing prostatic disease UTI’s become much more common.
UTI is a non-specific term and may refer to a number of conditions including asymptomatic bacteriuria, urethritis, cystitis, and pyelonephritis (infected kidney). Patients with pyelonephritis are at risk of bacteraemia and sepsis and therefore need rapid treatment with appropriate antibiotics
Causative Agents = GI Organisms
· E.coli (commonest), Klebsiella, Proteus, Enterobacter, Pseudomonas spp
Clinical Features
Symptoms
Chills and rigors are common. Fatigue. Malaise
Pain
usually in the affected flank or costovertebral angle +/- suprapubic. Pelvic or Perineal dysuria.
GU Symptoms
dysuria, frequency, urgency, passing small volumes
GI Symptoms
Nausea + Vomiting is common, diarrhoea
Elderly patients
May present with non specific signs e.g. decreased appetite, decreased mobility, increase confusion, lethargy etc
Signs
Signs of Sepsis
Fever, Tachycardia, Hypotension, tachypnoea
Abdomen
Flank, costovertebral or suprapubic tenderness
Sexually active women – may warrant a pelvic exam if ? PID.
PV discharge, adnexal tenderness, cervical excitation
Men may warrant PR exam
looking for tender prostate = prostatitis
Differential Diagnosis
Urinary
cystitis
renal colic
infected obstructed kidney
Bowel
Diverticulitis
Colitis
Appendicitis
Inflammatory bowel disease
Female
Pelvic Inflammatory Disease
Septic abortion
Ovarian cyst
Tubo-ovarian abscess
Biliary
Cholecystitis
Cholelithiasis
Choledocholithiasis
Cholangitis
Male
Prostatitis
Respiratory
Lower lobe pneumonia
Empyema
PE
Clinical Investigations
Bedside
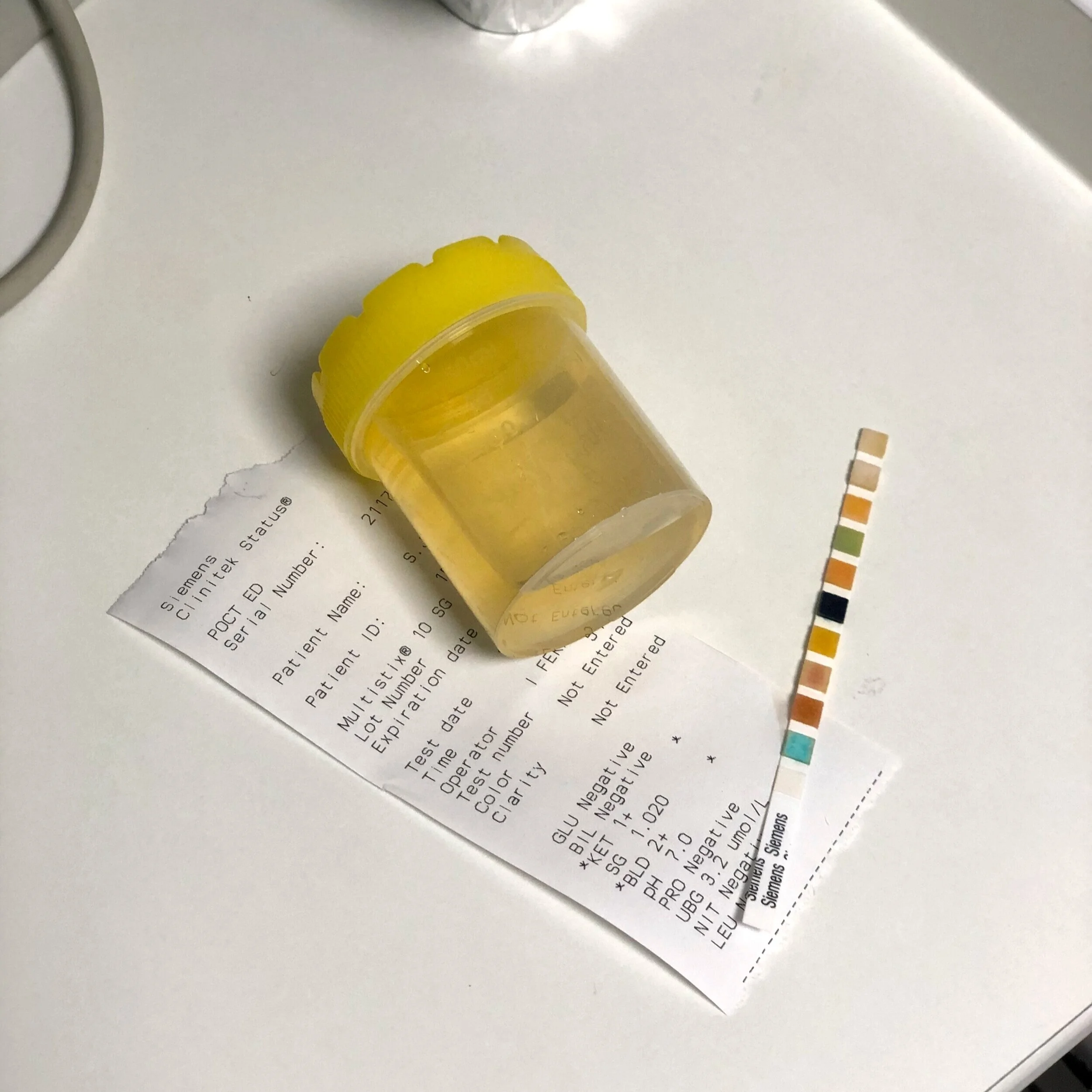
Urinalysis
Presence of leucocytes = PPV 50%, NPV 92%,
Nitrites = +ve if Gram Negative infection. High PPV. Low NPV as nitrites not produced by Gram +ve bacteria, enterococcus + pseudomonas
Urinary BHCG in all women of child bearing age
VBG – if concerned re sepsis.
POCUS – experienced operator. Looking for hydronephrosis or signs of pyelonephritis
Laboratory
MSU
WCC > 10,000 = Pyuria
Urine Culture
Blood Culture if concerned for Sepsis
FBC – High WCC,
CRP – elevated
U&E -? AKI if dehydrated, septic, obstructed
LFT + Amylase – out rule other causes
Radiology
Imaging not indicated in mild cases
Renal Ultrasound
normal in 75% cases of pyelonephritis but useful in showing complications e.g. abscess, hydronephrosis, renal infarction
CT
more sensitive especially if concerned regarding stone or obstruction
Management and Disposition
** Don’t forget the Sepsis 6 within 1 hour of presentation
Initial Resuscitation
IV Fluids as clinically indicated
If evidence of sepsis titrate to U/O, BP and lactate.
Consider IV vasopressor if severe sepsis and no response to initial fluid resuscitation
Specific Treatment
Antibiotics as per local guidelines
E.g.
Uncomplicated Cystitis = Nitrofurantoin 50mg QDS PO x 1/52
Recent Treatment/Hospitalisation = Co-amoxiclav 625mg PO TDS x 1/52
Pyelonephritis = Co-amoxiclav 1.2g IV TDS + Amikacin 15mg/kg IV
Symptomatic Treatment
IV Analgesia and anti-emetic as indicated
Antipyretic if patient significantly symptomatic with fever
Disposition
Mild cases of pyelonephritis can be managed in the community with PO antibiotics.
If vomiting or systemically unwell/signs of sepsis patient needs to be admitted medically for intravenous antibiotics and IV fluids
References
1. Cameron et al. Textbook of Adult Emergency Medicine 4th Edition. Chapter 9.4 Urinary Tract Infections
2. https://radiopaedia.org/articles/acute-pyelonephritis-1?lang=us
3. SJH Prescribers Capsule. Empiric antimicrobial guidelines. Genitourinary
4. Case courtesy of Assoc Prof Frank Gaillard, Radiopaedia.org, rID: 28838
This blog post was written by Dr Deirdre Glynn and was last updated in October 2020