Anticholinergic Syndrome
Introduction
Anticholinergic syndrome occurs secondary to the inhibition of central and peripheral acetylcholine muscarinic receptors.
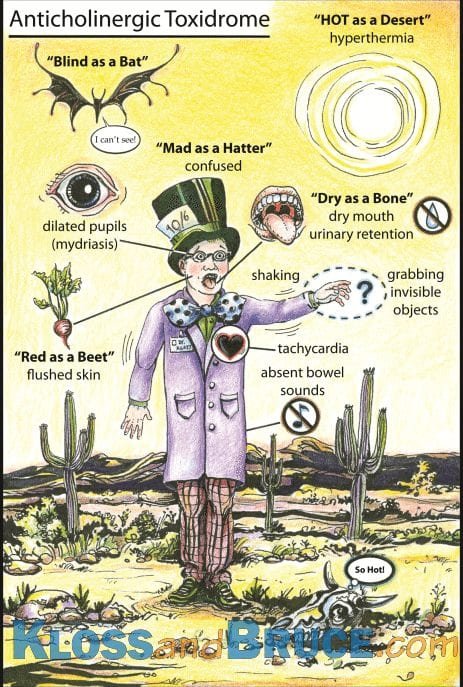
Central inhibition leads to a hyperactive delirium - typically including confusion, restlessness and picking at imaginary objects - which characterises this toxidrome. Peripheral inhibition is variable but symptoms may include hot, dry skin, facial flushing, mydriasis, tachycardia and urinary retention.
There is a spectrum of severity ranging from mild to life threatening presentations. However, as many anti-cholinergic drugs are “dirty” drugs that are active at numerous receptors and ion channels, seizures, coma and cardiovascular toxicity may not be secondary to anticholinergic effects and rather be secondary to drug effects on other receptors e.g. TCAs.
Anticholinergic Agent Examples
Antidepressants
Tricyclic Antidepressants (TCAs)
First Generation Antipsychotics
Haloperidol, Prochlorperazine (Stemetil), Chlorpromazine
Atypical Antipsychotics
Olanzapine, Quetiapine
Anticonvulsants
Carbamazepine
Antihistamines
Promethazine (Phenergan), Chlorpheniramine (Piriton)
Antimuscarinics
Atropine, Glycopyrrolate, Hyoscine
Antiparkinsons
Benztropine, Amantadine
Plants + Herbs
Some mushrooms, Dartura spp
Clinical Features
Symptoms
Hot, thirsty, confusion, blurred vision
Signs
Central – Agitated delirium (may last days), Tremor, Hyperthermia, Coma, Seizures (rare)
Peripheral = Dry skin, Dry mouth, Mydriasis, Facial Flushing, Tachycardic, Decreased bowel sounds, Urinary retention
NB actively look for evidence of urinary retention in these patients. Their confusion may limit their ability to communicate. Urinary retention may further exacerbate their delirium.
Differential Diagnosis
Infective
Sepsis from any source
Metabolic
Hyponatraemia
Hepatic Encephalopathy
Clinical Investigations
ALL Toxicology presentations should have:
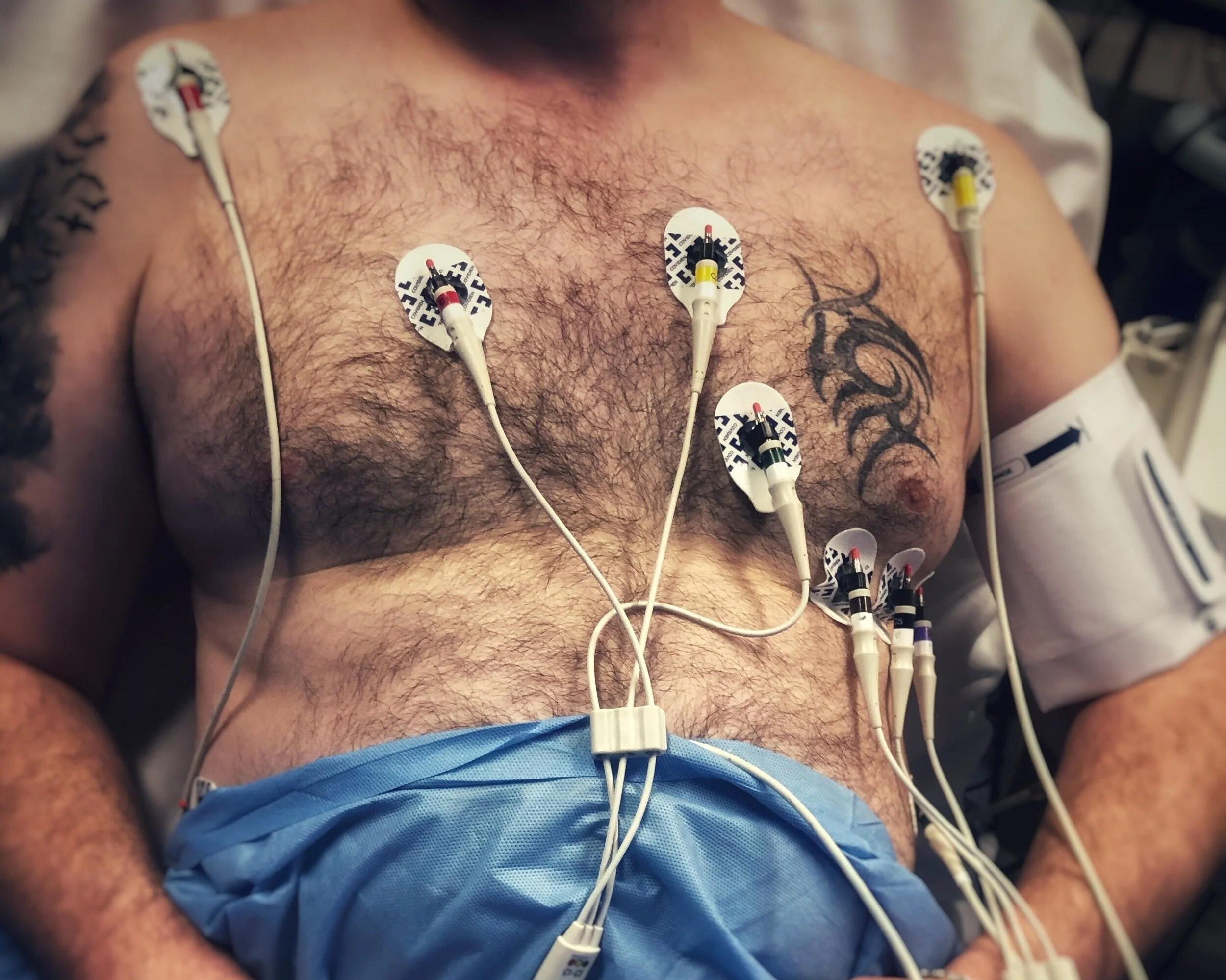
ECG
sinus tachycardia
look for signs of conduction disturbance indicating Na or K channel blockade.
Venous Blood Gas
Blood Sugar
Urine BHCG in females <50yrs
Serum paracetamol if any concerns
U&E, LFTs
assess for evidence of end organ damage secondary to OD or pre-exiting impairment which may affect drug clearance
CK
? Rhabdomyolysis
CXR
assess for evidence of aspiration
CT Brain
may be be necessary as part of the delirium work up
Management & Disposition
Resuscitation
Attention to airway, breathing and circulation as clinically indicated.
Treat seizures with IV benzodiazepines
No role for IV antiepileptics in toxic seizures
Seek and treat hypoglycaemia
Seek and treat hyperthermia
IV fluid to treat deficit and maintenance. Patients may be dehydrated at presentation and are often unable drink due to agitation
Specific Treatment
Physostigmine
A centrally acting acetylcholinesterase inhibitor that may have some role in controlling delirium in isolated anti-cholinergic agent toxicity (i.e. Not for use in polypharmacy OD or “dirty” drug OD)
Has a short half life, multiple adverse effects and contra-indications so supportive treatment is preferred.
Supportive Treatment
Supportive treatment is the mainstay of treatment
Reassure. Manage in a quiet area. One to one nursing care is often necessary to frequently reorientate the patient.
In dwelling catheter for urinary retention
Treat agitation with PO or IV Diazepam (long acting).
Repeat doses are often required but avoid oversedation
Avoid drugs with known anticholinergic effects e.g. haloperidol
Disposition
Once established it is difficult to predict the duration of delirium. It may persist for several days depending on the agent involved
These patients are best admitted under a medical team for ongoing supportive management and nursing
References
Murray et al. Toxicology Handbook. 2nd edition
www.rch.org.au/clinicalguide/guidelineindex/Anticholinergic_Syndrome/
Graphic by Dr Brian Kloss. www.klossandbruce.com
Dunn et al. The Emergency Medicine Manual. 5th Edition. Volume 2
This blog was written by Dr Deirdre Glynn and was last updated on April 13th 2022