Cardiogenic Shock
Introduction
Cardiogenic shock is failure of cardiac contractility which leads inadequate organ perfusion and oxygen delivery to tissues. It is clinically defined as SBP < 90mmHg or MAP > 30mmHg below baseline for > 30 mins
The most common cause of Cardiogenic Shock is Acute Myocardial Infarction causing LV failure. Mortality in this group is up to 70%. Other causes include;
Tachyarrhythmias causing acute heart failure
Acute decompensation in cardiomyopathies or an acute cardiomyopathy
Acute Myocarditis
Myocardial Contusion
Acute Valve Failure
Severe Outflow Obstruction (e.g. Aortic Stenosis, HOCM)
Drug overdose (Beta Blockers, Calcium Channel Blockers)
Clinical Features
Symptoms
Cardiovascular
chest pain, palpitations, diaphoresis, fatigue
Respiratory
SOB, cough productive of pink frothy sputum.
Signs
Signs of shock
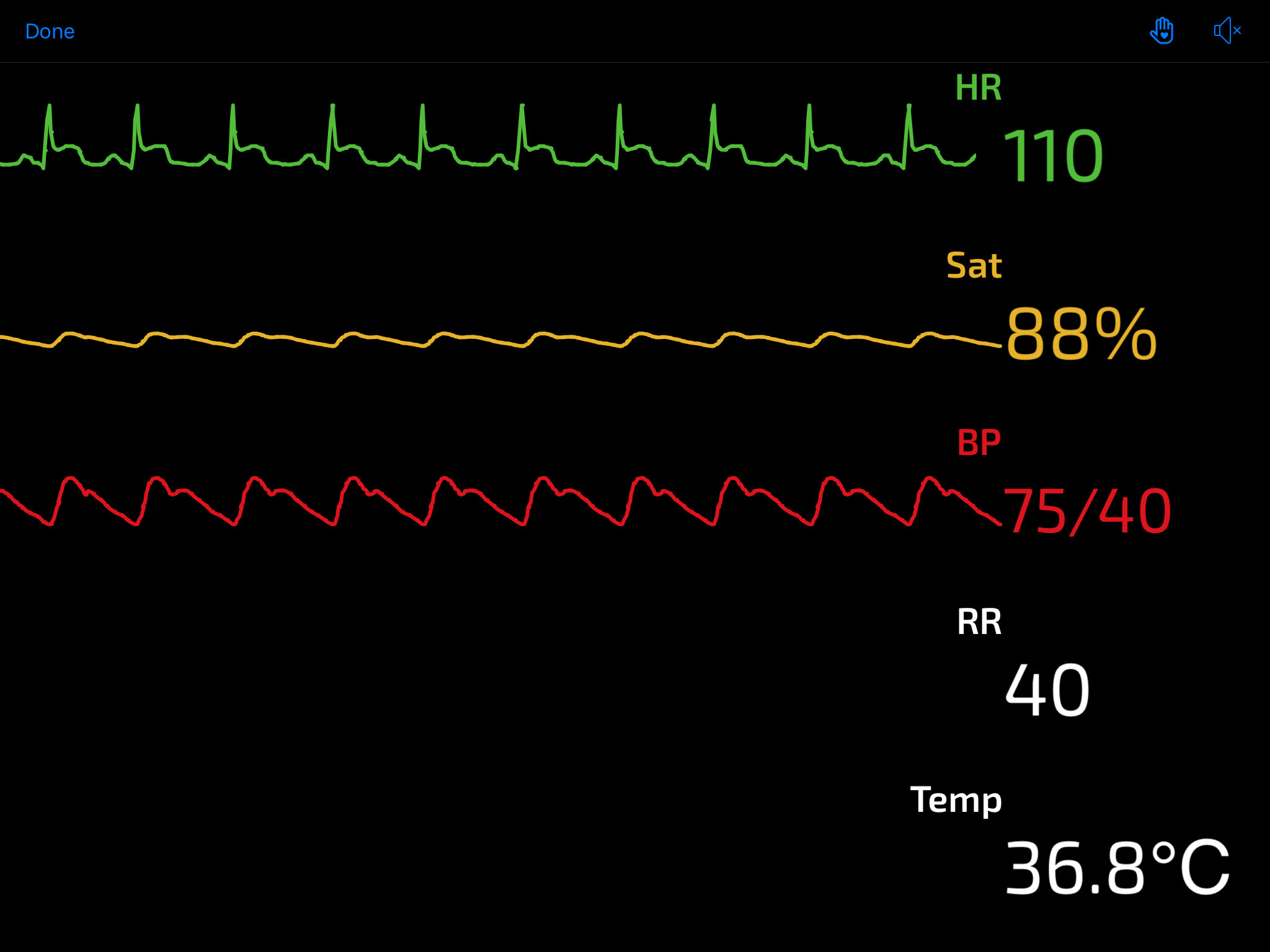
Tachycardia, hypotension, pallor, hypoxia, delayed CRT, decreased U/O
Signs of heart failure
Tachypnoea, bilateral crackles, gallop rhythm, raised JVP, peripheral oedema
Differential Diagnosis
Other Causes of Shock
Hypovolaemic Shock
Obstructive Shock
e.g. Cardiac tamponade, massive PE, tension pneumothorax
Clinical Investigations
Bedside
ECG
assessing for presence of ST elevation + territory, presence of heart block
VBG
Low pH and high lactate indicating end organ hypoperfusion
POCUS
Echo – assessing for LV dilatation, LV Dysfunction. Dilated IVC
Lung US – presence of bilateral B lines consistent with pulmonary oedema, pleural effusions
Laboratory
FBC, U&E, LFT, CRP
baseline bloods and seeking other causes
Troponin
Baseline Coag
Radiology
CXR – cardiomegaly and findings consistent with pulm oedema. (ABCDE)
Alveolar Oedema
Kerley B Lines
Cardiomegaly
Dilated upper lobe vessels
Pleural Effusion
Formal Echocardiography
quantitative assessment of LV, RV and all valves
Coronary Angiogram
to seek and treat coronary artery disease causing myocardial ischaemia
Management & Disposition
Initial Resuscitation
Patient should be managed in a resus environment with immediate attention to any ABC issues.
O2 Therapy as required.
Patient may require Positive End Expiratory Pressure (PEEP) to maintain oxygenation. This can be administered non invasively (i.e. CPAP/BiPAP) or invasively (i.e. intubation)
Hypovolaemia should be looked for and if present treated with cautious alliquots of 250ml of crystalloid.
Fluids also NB if RV infarction in inferior STEMI to maintain preload
Persistent hypotension and shock is best treated with emergency revascularisation in the cath lab.
In the meantime or if nothing to stent patient should have CVC inserted and be commenced on inotropes e.g. noradrenaline, dobutamine
Specific Treatment
Emergency revascularization with PCI or CABG is the most important treatment and offers the best chance of survival to patients with AMI
Load with dual antiplatalets
e.g. Aspirin 300mg PO + Ticegralor 180mg PO in ED
STEMI patients in centre without access to primary PCI should be thrombolysed if early transfer to PCI centre is not available
Symptomatic Treatment
IV analgesia by titrated opioids as required.
Disposition
STEMI or Critical ischaemia patients = Urgent transfer to cath lab under cardiology
If other cause for cardiogenic shock patient should be admitted to ICU for ongoing inotropic treatment and organ support as required.
References
1. Garrett P, Cameron P. Shock Overview. Textbook of Adult Emergency Medicine. 4th Edition.
2. Case courtesy of Dr Tomas Jurevicius, Radiopaedia.org, rID: 48089
This blog was written by Dr Deirdre Glynn and was last updated in December 2020



