Anaphylactic Shock/Anaphylaxis
Introduction
Anaphylaxis is a serious allergic reaction that is rapid in onset following exposure to a trigger and may cause death. It is a medical emergency that requires immediate diagnosis and treatment.
The most common causes are drugs (e.g. Penicillin, Aspirin, NSAIDs), insect stings (bees, wasps, ants) and food (nuts, eggs, shellfish). Sometimes no cause is readily identifiable
Clinical Features
Symptoms
Skin
tingling or warmth, flushing, itch
Respiratory
throat tightness, cough, hoarseness, SOB
Cardiovascular
dizzy, chest pain
Gastrointestinal
Cramps, diarrhoea, Nausea, vomiting
General
anxiety, impending sense of doom, confusion
Signs
Signs of Shock
loss of airway, reduced GCS, hypoxia, tachypnoea, hypotension, tachycardia, pallor, diaphoresis
Respiratory
Stridor, drooling, hoarseness, tachypnoea, wheeze, cyanosis, apnoea
Cardiovascular
hypotension, tachycardia, syncope, arrhythmia, cardiac arrest
Skin
angio-oedema of any site, erythema, urticaria
Clinical Criteria for Anaphylaxis
Anaphylaxis is highly likely when any 1 of the 3 criteria below occur
1. Acute onset of illness with involvement of skin or mucosa (swelling, rash) and one of;
a. Respiratory compromise
b. Reduced BP or other evidence of end organ hypo-perfusion e.g. syncope
2. 2 or more of the following occurring rapidly after exposure to likely allergen
a. Involvement of skin or mucosa
b. Respiratory compromise
c. Hypotension or evidence of same e.g. syncope, incontinence
d. Persistent GI symptoms e.g. nausea, vomiting, diarrhoea
3. Hypotension after exposure to known allergen for patient
Differential Diagnosis
Allergic Reaction not fulfilling anaphylaxis criteria
Other forms of shock
septic shock, cardiogenic shock, hypovolaemic/haemorrhagic shock, obstructive shock
Wheeze/SOB
Asthma, pulmonary oedema, pneumothorax, infection
vasovagal, cardiogenic syncope, neurogenic syncope
Angio-oedema
C1 esterase deficiency, Drug induced angio-oedema (e.g. ACEi)
Clinical Investigations
Anaphylaxis is a clinical diagnosis. No investigations are necessary and should not delay treatment.
Patient should have baseline bloods and ECG once treatment commenced. Other investigations may be warranted if diagnosis is in doubt.
Bedside
VBG, ECG
Laboratory
FBC, U&E, May be role for Tryptase level in follow up
Radiology
CXR if concerned for pulmonary oedema, pneumothorax or infection
Management & Disposition
Initial Resuscitation
Single most important treatment is rapid administration of Adrenaline
500mcg IM Adrenaline repeated every 5-10 mins according to response or relapse
If cardiovascular collapse and patient has IV access or if patient refractory to IM adrenaline an IV adrenaline infusion should be commenced
Following administration of Adrenaline securing airway is next priority
If airway oedema patient will be a difficult airway ++. Call for help
Nebulised adrenaline if airway oedema
High Flow O2
IV crystalloid if hypotensive post adrenaline
Decontamination i.e. remove any allergen that may still be on patient/in patients mouth/in patients cannula.
Second Line Treatment
Little evidence but may have some role in controlling symptoms e.g. itch and preventing recurrence (Biphasic reaction)
IV Anti-histamine – rash, itch
IV Hydrocortisone – rash, itch, prevent biphasic reaction
Salbutamol Nebuliser – SOB, Wheeze
Disposition
Any patient who receives adrenaline should be closely observed in ED for 4-6 hours
If the patient needs > 1 dose of adrenaline they should be admitted for observation
If patient needs intubation or adrenaline infusion they need to be admitted to ICU
Prior to discharge
Patient and family needs to be educated regarding the importance of avoiding relevant allergen.
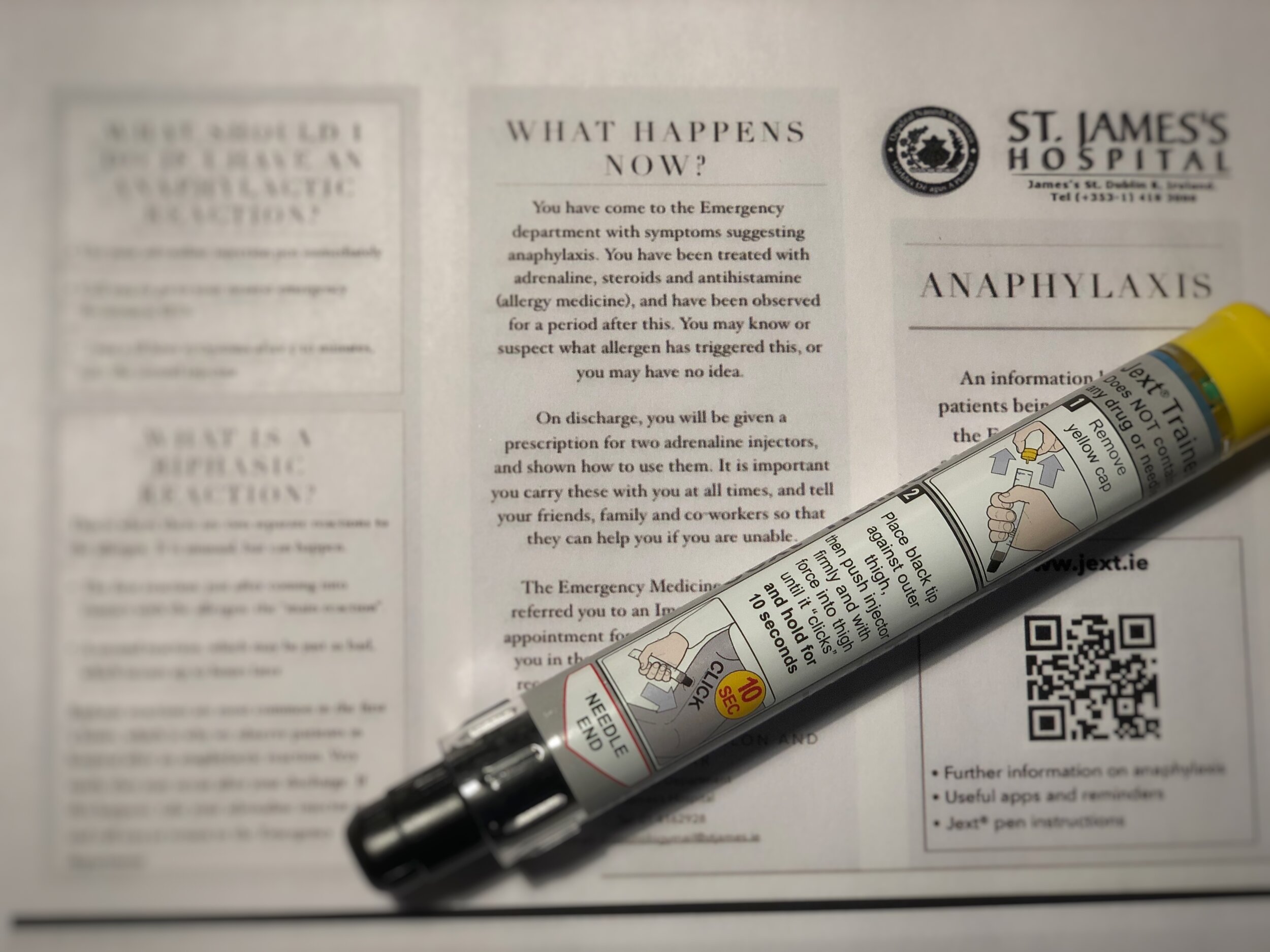
Patient needs to be prescribed 2 x adrenaline auto-injectors e.g. Jext, Epipen. They and their family members need to be educated on how AND when to use them
https://adults.jext.co.uk/about-jext/how-to-use/
http://www.epipen.ie/your-epipenr-adrenaline-auto-injector/epipen-user-guide/
References
Tintanelli et al. Chapter 27 Anaphylaxis, Acute Allergic Reactions and Angio-oedema. Emergency Medicine, A Comprehensive Study Guide. 7th Edition
Brown A, Cameron P. Anaphylaxis. Textbook of Adult Emergency Medicine. 4th Edition
Rice M. St James’s Hospital Emergency Department - Anaphylaxis Integrated care pathway. July 2020
This blog was written by Dr Deirdre Glynn and was last updated in November 2020

