Septic Shock
Introduction
Septic shock is an emergency life threatening condition. It has an in hospital mortality in Ireland of 40%.
Sepsis exists on a continuum of severity.
Signs of End Organ Dysfunction
New O2 requirement to keep sats > 90%
SBP < 90mmHg
New altered mental status
Lacate > 4 post fluids
Bilirubin > 32
Platalets < 100
Oliguria or Anuria despite fluids
New AKI. Creat > 170
Risk Factors for Developing Sepsis
Age > 75 yrs
Frailty
Significiant comorbidities
COPD, Cancer, HIV/AIDS, DM, CKD, Chronic Liver Disease
Immunosupressant medications
Recent Surgery/Major trauma
Clinical Features
Symptoms
Feeling hot and cold, lethargy, weakness/collapse
Symptoms suggesting source e.g. headache, limb swelling, cough, diarrhoea, abdo pain, urinary symptoms
Signs
Appearance
pale, sweaty, mottled, cold or hot to touch
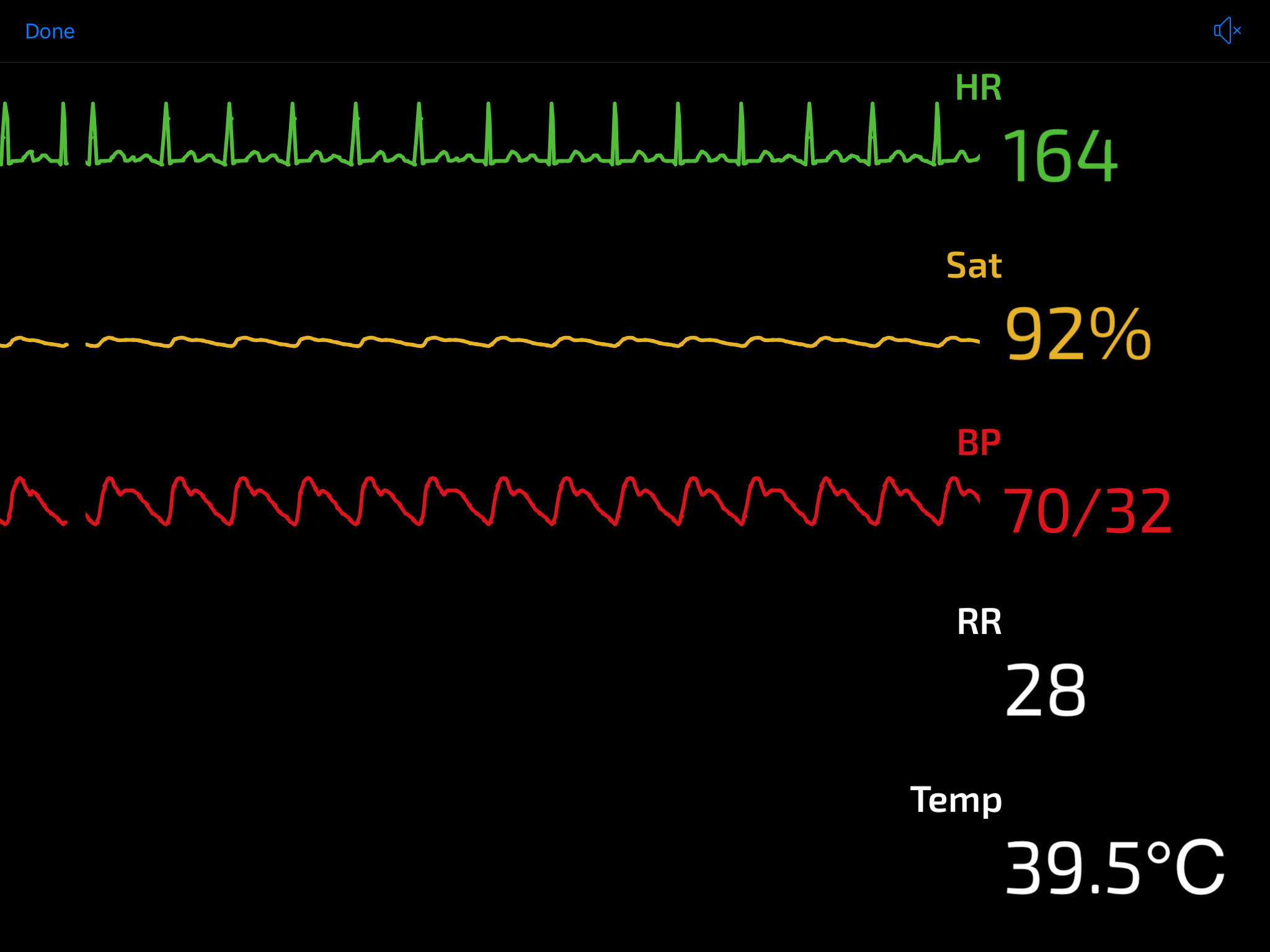
Abnormal vitals
Tachycardia, Tachypnoea, Hypoxia, Hypo/Hyperthermia, Hypotension
Altered conscious state
Signs indicating source of infection
Meningitis – rash, neck stiffness, Kernigs + Brudzinksi’s sign
Chest – Crackles, wheeze
Abdomen – tenderness, diarrhoea, distension
Urinary – flank tenderness
Skin/Soft tissue – swelling, erythema, tenderness
Differential Diagnosis
Other causes of shock
Other causes of SIRS and vasodilatory or distributive shock e.g. Pancreatitis, Burns, Toxicology
Hypovolaemic/Haemorrhagic Shock
Obstructive shock e.g. PE, Cardiac Tamponade
Clinical Investigations
Bedside
VBG
high lactate = evidence of end organ dysfxn, Metabolic acidosis concerning for hypoperfusion, Abn electrolytes/Hb, High or low BM
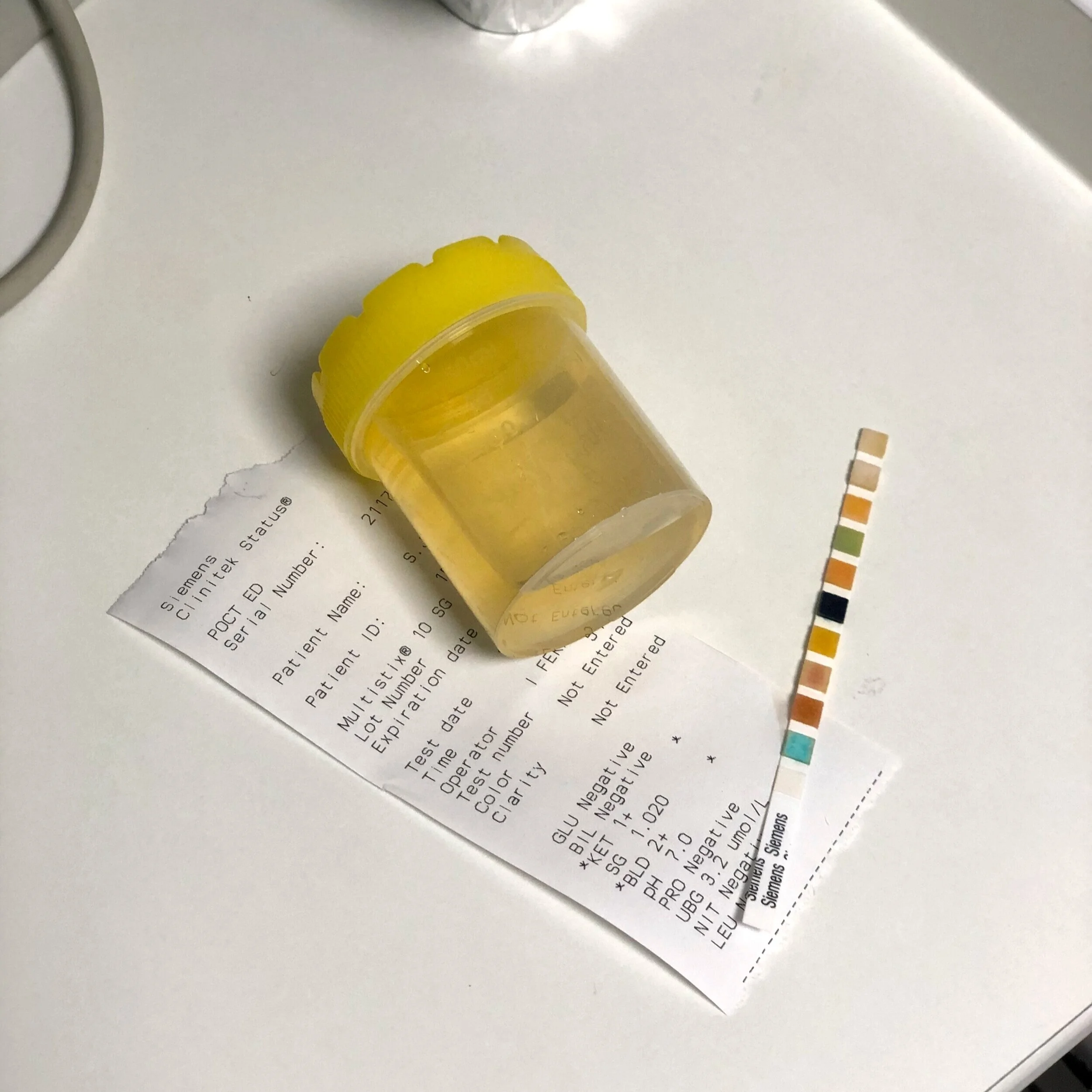
Urinalysis
? urinary source
Urinary BHCG if female + of child bearing age.
ECG
looking for evidence of ACS
POCUS
Cardiac US can outrule other causes of shock, ? AAA, ? Peritoneal free fluid i.e. RUSH exam.
Laboratory
Blood Cultures prior to abx.
Peripheral cultures and cultures from any central lines/ports.
FBC
high/low WCC, Low Plts
U&E
evidence of AKI or electrolyte abn
LFT
? elevated bili. ? Derangement indicating possible source
Amylase
if pancreatitis in differential
CRP
Elevated. Not necessary to make diagnosis but can be useful to monitor trend
CoAg
may be deranged indicating end organ dysfxn
Radiology
CXR
? chest source. If normal doesn’t out rule pneumonia as CXR findings can lag behind clinical
US and CT scan depending on likely source
Management and Disposition
Anyone who you think may have Sepsis, Severe Sepsis or Septic Shock needs to have the Sepsis 6 within 1 hour
Initial Resuscitation
Attention to airway and breathing as clinically indicated
IV Crystaloid as clinically indicated
Titrate to BP, U/O and lactate
Remeasure lactate post fluid resus
Initial fluid resus is typically 2 L in the first hour unless fluid intolerant e.g. Pulmonary oedema
Continuous monitoring of vitals including urine output
MAP < 65 and Lactate > 2 following fluid resuscitation = Septic Shock
Consider Inotropes i.e. Noradrenaline infusion + critical care transfer
Specific Treatment
IV Antimicrobials based on local guidelines depending on suspected source
i.e. CAP, HAP, Skin + soft tissue, Urinary, Meningoencephalitis, Intraabdominal, Neutropaenic sepsis, Sepsis of unknown origin
Source control
e.g. infected obstructed kidney needs nephrostomy, Intra-abdo source may require surgery, abscesses need to be drained etc.
Symptomatic Treatment
IV analgesia and anti-emetic as required
Anti-pyretic if patient symptomatic with fever.
Do not use antipyretic agents with the sole aim or reducing body temperature
Disposition
Any patient with sepsis needs to be admitted to the hospital.
Admitting team depends on likely source
Septic Shock needs to be admitted to HDU/ICU for vasopressors +/- other organ supports
References
2. SJH Emergency Department Sepsis assessment and management proforma
This blog post was written by Dr. Deirdre Glynn and was last updated in October 2020